Paracervical local anaesthesia for cervical dilatation and uterine interventions

PARACERVICAL BLOCK anesthesia is a simple, safe and effective means
of relieving pain eliminates the need for depressing amounts of analgesic drugs. It involves injection of local anaesthetic around the cervix to numb nearby nerves. Cervical dilatation and uterine interventions such as: -hysteroscopy,endometrial biopsies, fractional curettage, and suction terminations, they can be performed without any analgesia or anaesthesia; with regional anaesthetic injections as with paracervical block; using oral or intravenous analgesics and sedatives; or under general anaesthesia. Many gynaecologists use paracervical block for uterine intervention
No serious maternal or fetal complications have been reported.
The principal use of paracervical block anesthesia is in relieving the pain of the first stage
of labor ,dilatation and curettage and in patients with an incomplete abortion where the relief it affords is quicker and
greater than that produced by drugs which act
on the central nervous system.
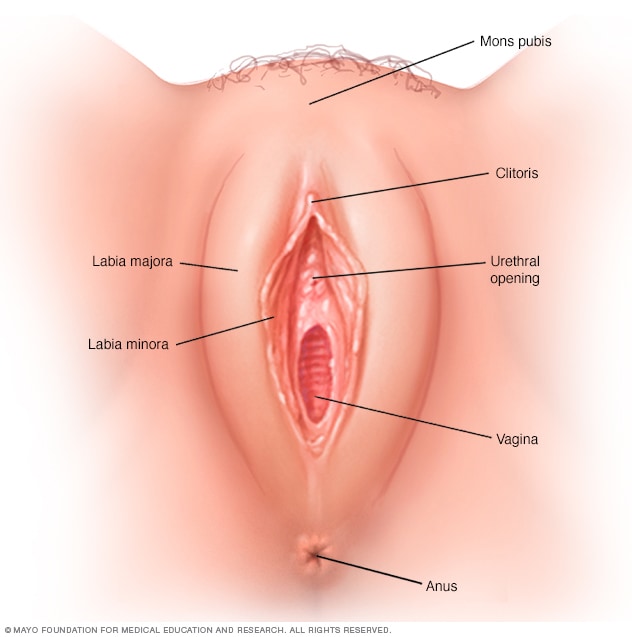
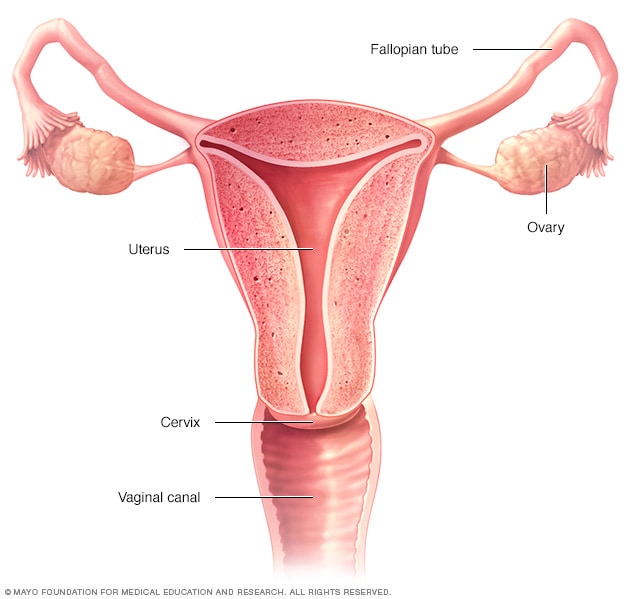
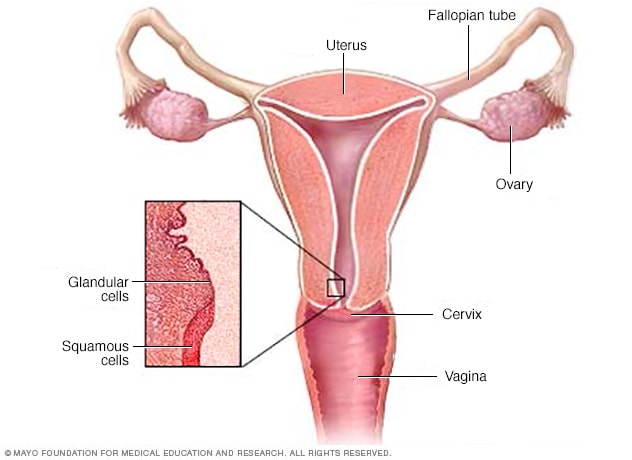
Neuroanatomy
First stage labor pain is due mainly to dilatation
of the cervix and to a lesser degree to uterine
contractions.3 The sensation of pain is due to
impulses passing by sensory and sympathetic nerve
pathways down the lateral and posterior portions
of the cervix into the area of the uterosacral ligaments. The impulses travel through the uterine,
pelvic and hypogastric plexuses into the lumbar
and lower thoracic chain to the rami of the eleventh and twelfth thoracic nerves to reach the spinal
cord. This route has been substantiated clinically
by the complete relief of pain afforded when spinal,
caudal, epidural, upper lumbar sympathetic, lower
thoracic, paravertebral, uterosacral or paracervical
block is used.
Pain of the second stage is produced primarily
by distension of the lower birth canal, vulva and
perineum and is conveyed by sensory pathways
of the pudendal nerves, which enter the spinal
cord via the posterior roots of the second, third
and fourth sacral nerves. Paracervical block, therefore, is not sufficient for delivery.
Procedure
Most anesthesiologists feel that any anesthesia,
even a local anesthesia, works more smoothly if
premedication is used. This is true with the paracervical block. I use meperidine hydrochloride
(Demerol®), promethazine hydrochloride (Phenergan®) and occasionally secobarbital sodium
(Seconal®). They are unnecessary after the block.
The Brittain Transvaginal Needle Guide* facilitates injection. This is a stainless steel tube with
a ball on one end to prevent injury to maternal tissues and a funnel on the other end to allow easy
access for the 6-inch 20-gauge needle. The needle
protrudes from the guide only 7 mm. This eliminates the danger of too deep an injection and
reduces the danger of hematoma formation to nil.
The block is performed with the patient in bed
under sterile drapes but without surgical preparation. The cervicovaginal fornix is located with
the examining finger and the guide is placed at
the 5 o'clock and 7 o'clock positions (Figure 1).
It is important to sweep the guide away from the
cervix in order to get into the posterior lateral
fornix. The needle is then inserted through the
guide, aspiration is made and the solution injected.
I use chiefly a 1 per cent solution of lidocaine
hydrochloride with epinephrine 1:1,000,000. This
is prepared by mixing 50 ml plain 1 per cent lidocaine with 5 ml 1 per cent lidocaine with epinephrine 1:100,000. Epinephrine is contraindicated in the presence of diseases such as diabetes,
hyperthyroidism, peripheral vascular disease, hypertension, nephritis and cardiac disease. The
addition of epinephrine makes the mixture much
safer than plain lidocaine hydrochloride and allows a longer duration of effect, but at the expense
of uterine inertia in a certain proportion of cases,
sometimes requiring use of an oxytocic agent. The
usual dosage of anesthetic agent is 8 to 10 ml on
each side. The maximum dosage is 50 ml-that
is, 500 mg of lidocaine hydrochloride with epinephrine. Only 300 mg is allowed without epinephrine.
If complete anesthesia is not obtained within
two or three contractions, 5 ml is repeated on
either or both sides. Sometimes there remains an
unanesthetized coin area in the lower abdomen
on one or both sides. This can be anesthetized
by injection of 5 ml at the 10 o'clock or the 2
o'clock position. I keep one guide curved to allow
easier introduction to these anterior locations.
Failure is unacceptable. Repeated efforts should
be made until the desired effect is achieved, but
with care to stay within the limits of safe dosage.
It must be emphasized that the greatest danger is
overdosage.
The block is given in the accelerated phase of
labor, usually at about 5 cm cervical dilatation.
Using lidocaine hydrochloride with epinephrine,
the duration of anesthesia is approximately one
hour and twenty minutes.
The quality of uterine contractions after the
block might seem poor and yet the progress in cervical dilatation be dramatic. This is because
the cervix has become so soft and free of tone
that even the mild contractions lead rapidly to
complete dilatation. Because of atonicity, cervical
lacerations are rare.
We have done over four thousand blocks using
this material in private practice. There have been
no serious maternal complications. An occasional
patient has complained of feeling faint or apprehensive from too rapid absorption, but these complaints have been very transient. Temporary numbness of one or both legs noted by some patients,
disappears as the paracervical anesthesia abates.
There have been no instances of hematoma,
thrombosis, infection, hypersensitivity reaction
or lumbosacral plexus neuritis. The only untoward effect is fetal bradycardia, noted in 4.7
per cent of cases. This should not be viewed with
alarm; it is probably due to a vasovagal reflex,
and must be distinguished from fetal distress.
Infants have been delivered during the period of
bradycardia in some cases and after its disappearance in others, and in none of them has fetal depression been present. On the contrary, the
infants are breathing and crying before the delivery is completed. The important point, therefore,
is that a careful evaluation must be made to distinguish the cases of fetal bradycardia due to fetal
distress from the transient bradycardia observed
following paracervical anesthesia.
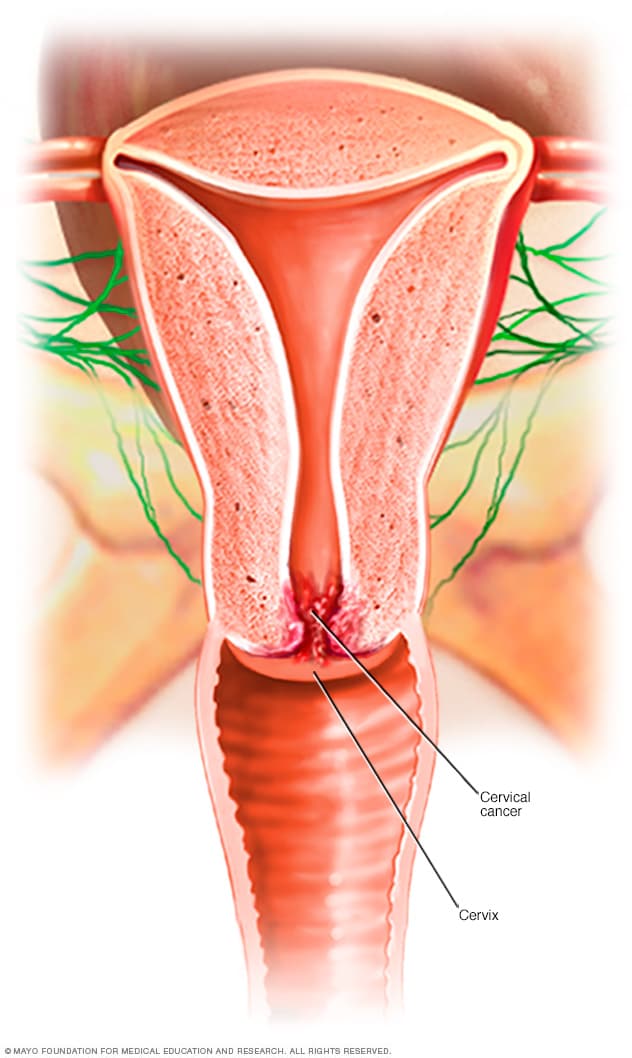
Gynecologic Use
Paracervical block for anesthesia for curettage is carried out without the Brittain Guide. A
3- or 4-inch 21-gauge needle is adequate, and
5 ml of the anesthetic solution is infiltrated at
the 4 o'clock position, 5 ml at 8 o'clock and
5 ml directly into each uterosacral ligament.
This provides the ideal anesthetic for completion of abortions and it is excellent for curettage
in many other circumstances. The method is not
recommended in the presence of vaginismus of
any cause. It is indicated where general anesthesia
or sophisticated forms of conduction anesthesia
are either unavailable or contraindicated. It is
especially useful if the patient has anemia, has too
recently eaten or has a respiratory problem or
is in borderline shock. Many patients with incomplete abortions fall into this category.
Paracervical block can also be used in other
minor procedures such as cervical repair, conization and Shirodkar or Wurm operations, although in such cases it is probably better to reserve it for the exceptionally poor risk patients.
Paracervical block has also been recommended
as an aid in the differential diagnosis of dysmenorrhea.
Book appointment today at Gyncentre : Email gyncentre@gmail.com Call / WhatsApp @ +254706666542