Overview
-
Cervical cancer
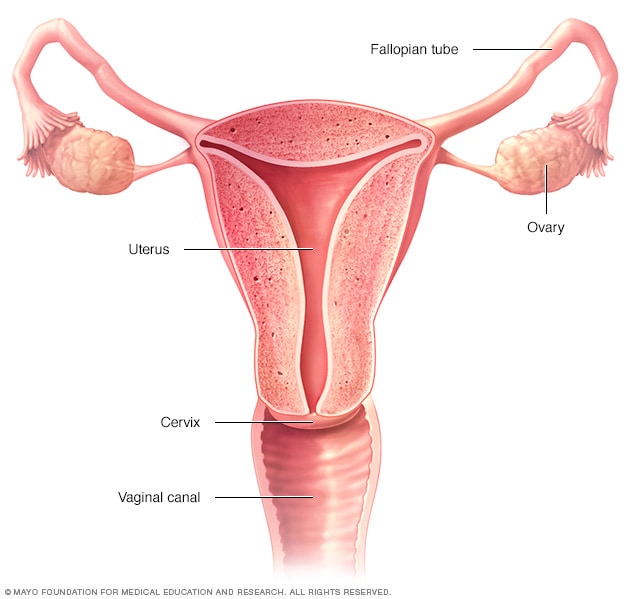
Cervical cancer is a type of cancer that occurs in the cells of the cervix — the lower part of the uterus that connects to the vagina.
Various strains of the human papillomavirus (HPV), a sexually transmitted infection, play a role in causing most cervical cancer.
When exposed to HPV, a woman's immune system typically prevents the virus from doing harm. In a small group of women, however, the virus survives for years, contributing to the process that causes some cells on the surface of the cervix to become cancer cells.
You can reduce your risk of developing cervical cancer by having screening tests and receiving a vaccine that protects against HPV infection.
Symptoms
-
Female reproductive system
Early-stage cervical cancer generally produces no signs or symptoms.
Signs and symptoms of more-advanced cervical cancer include:
- Vaginal bleeding after intercourse, between periods or after menopause
- Watery, bloody vaginal discharge that may be heavy and have a foul odor
- Pelvic pain or pain during intercourse
When to see a doctor
Make an appointment with your doctor if you have any signs or symptoms that concern you.
Causes
-
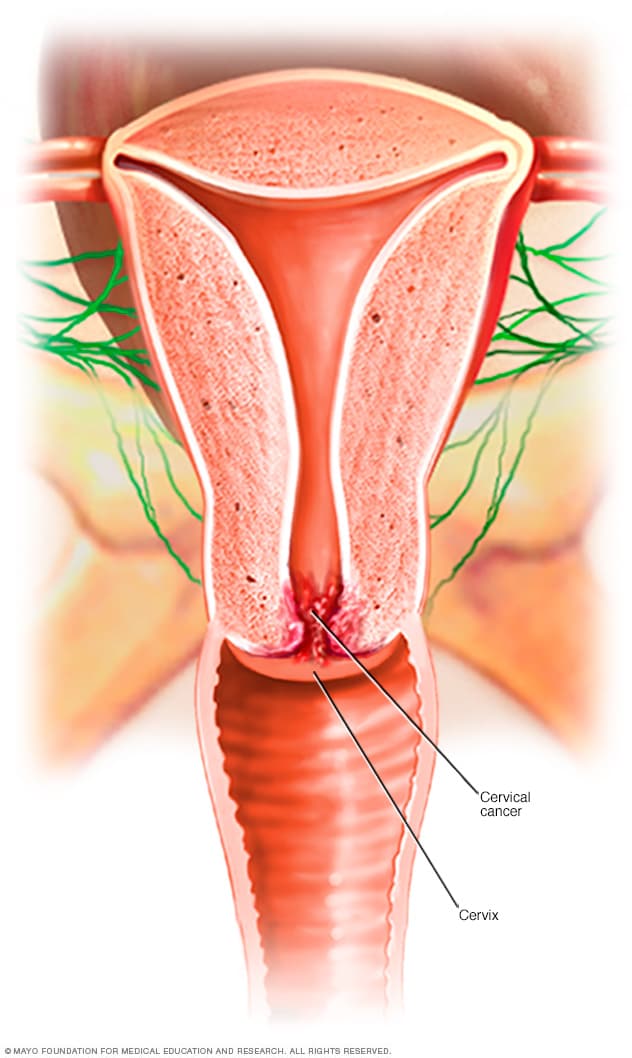
Where cervical cancer begins
Cervical cancer begins when healthy cells acquire a genetic change (mutation) that causes them to turn into abnormal cells.
Healthy cells grow and multiply at a set rate, eventually dying at a set time. Cancer cells grow and multiply out of control, and they don't die. The accumulating abnormal cells form a mass (tumor). Cancer cells invade nearby tissues and can break off from a tumor to spread (metastasize) elsewhere in the body.
It isn't clear what causes cervical cancer, but it's certain that HPV plays a role. HPV is very common, and most women with the virus never develop cervical cancer. This means other factors — such as your environment or your lifestyle choices — also determine whether you'll develop cervical cancer.
Types of cervical cancer
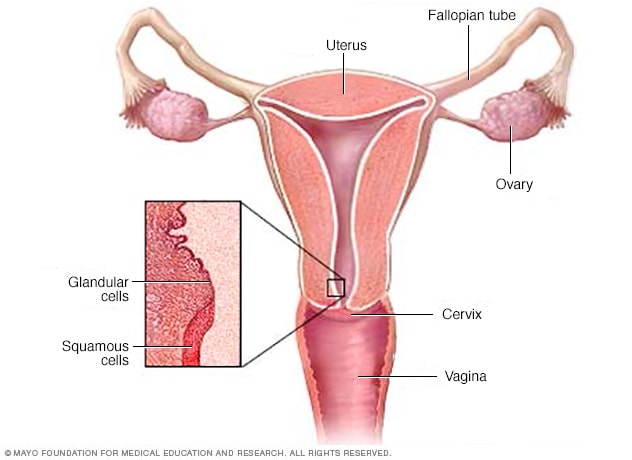
The type of cervical cancer that you have helps determine your prognosis and treatment. The main types of cervical cancer are:
- Squamous cell carcinoma. This type of cervical cancer begins in the thin, flat cells (squamous cells) lining the outer part of the cervix, which projects into the vagina. Most cervical cancers are squamous cell carcinomas.
- Adenocarcinoma. This type of cervical cancer begins in the column-shaped glandular cells that line the cervical canal.
Sometimes, both types of cells are involved in cervical cancer. Very rarely, cancer occurs in other cells in the cervix.
Risk factors
Risk factors for cervical cancer include:
- Many sexual partners. The greater your number of sexual partners — and the greater your partner's number of sexual partners — the greater your chance of acquiring HPV.
- Early sexual activity. Having sex at an early age increases your risk of HPV.
- Other sexually transmitted infections (STIs). Having other STIs — such as chlamydia, gonorrhea, syphilis and HIV/AIDS — increases your risk of HPV.
- A weak immune system. You may be more likely to develop cervical cancer if your immune system is weakened by another health condition and you have HPV.
- Smoking. Smoking is associated with squamous cell cervical cancer.
Prevention
To reduce your risk of cervical cancer:
- Get vaccinated against HPV.Vaccination is available for girls and women ages 9 to 26. The vaccine is most effective if given to girls before they become sexually active.
- Have routine Pap tests. Pap tests can detect precancerous conditions of the cervix, so they can be monitored or treated in order to prevent cervical cancer. Most medical organizations suggest women begin routine Pap tests at age 21 and repeat them every few years.
- Practice safe sex. Using a condom, having fewer sexual partners and delaying intercourse may reduce your risk of cervical cancer.
- Don't smoke.